May 15, 2019
The New York Times: 2019/05/13 “Stem cell Treatments Flourish with Little Evidence That They Work”
Several years ago, I asked a question of a cellular biologist as to how is Bone Marrow Concentrate effective if the number of adult mesenchymal stem cells diminish as we age? His response: “Bone Marrow contains lots of things including stem cells and proteins called cytokines or growth factors. It may be that the growth factors are most important in joint restoration and blocking pain.”
Let’s take for example, inflammatory arthritis such as Rheumatoid and Psoriatic arthritis. The common denominator is a pro-inflammatory cytokine called Tissue Necrosis Factor found in the body’s immune system. The growth factor, TNF-alpha blocker is now used to control the inflammation and alter the body’s immune response to the proinflammatory protein. As a result of TNF-alpha blockers, Phil Mickelson is a very competitive golf professional, (You have seen him as a spokes person for Psoriatic Arthritis treatment with Humira). Since the introduction of TNF alpha blockers in Scandinavia five years ago, there has been a 40% reduction in Total Knee Replacements for inflammatory arthritis. When Kobe Bryant traveled to Dusseldorf, Germany almost nine years ago, he received treatment for a very arthritic knee with Interleukin -1 Receptor Antagonist Protein, along with other blockers. Shortly thereafter, he returned to play another five years in the NBA. The IRAP that Bryant received was and is an anti-inflammatory, a growth factor blocker, a cytokine.
As I agree in part with the criticism in the New York Times concerning Stem Cells, those who read this Blog will recall that I don’t “sell” stem cells. Bone Marrow is used in part because of the fact that it contains stem cells; but more importantly as we age, Bone Marrow contains Growth Factors, the anti-inflammatory protein Cytokines that restore a joint by minimizing pain and improving function. Over the last eight years, we have accumulated the evidence that Bone Marrow Concentrate works for arthritis via stem cells, growth factors, or all of the above. Recently we have taken a major step forward by filtering high concentrations of Growth Factors from the Platelet Poor Plasma, previously discarded, that remained after we centrifuge the bone marrow and add the filtrate to that which is injected into the painful joint. Stem Cells maybe, highly concentrated Growth Factors that act to block pain and improve function, for certain.
You may learn more by visiting my web site at www.sheinkopmd.com or call for a consultation (847)390-7666
Tags: ACL, ACL Injury, anterior cruciate, arthritic knee, arthritis, Autologous Protein Concentrate, BMC, board-certified, Bone Marrow Concentrate, bone marrow edema, cells, cellular orthopedic, cellular orthopedics, FDA, Growth Factors, hematopoietic cell, inflammatory arthritis, injection, Interleukin 1 Receptor Antagonist Protein, IRAP, joint health, joint pain, knee replacement, Kobe Bryant, meniscal injury, meniscectomy, Mesenchymal Stem Cell, micro-fragmented adipose, muscle injury, muscle strain, nterleukin -1 Receptor Antagonist Protein, OA, Orthopedic Surgeon, Osteoarthritis, pain, Physical Therapy, Platelet Rich Plasma, platelets, pro-inflammatory cytokine, PRP, Psoriatic Arthritis, regenerative medicine, repair, Rotator cuff tear, sports injuries, sports medicine, stem cells, strain, tear, Tissue Necrosis Factor, TNF alpha blocker, torn medial meniscus, training
Apr 11, 2019
I consider myself an aging athlete who still skis, cycles, dedicates five days a week to fitness, plans to soon plant a garden, and walks up a spring creek with a fly rod. When my arthritic hips and knees began to limit my recreational profile several years ago, I chose the regenerative medicine option rather than joint replacements. Having performed joint replacements for 37 years and studied the benefits and limitations of such, I elected to postpone, perhaps avoid major surgery with the inherent risks and limitations. First it was Platelet rich plasma, next came PRP with Growth factor Proteins; and next came stem cells. At the get go, I did not expect to regenerate cartilage; but I did hope to restore joint function, minimize pain, and maintain the highest possible activity potential. Even with Grade 4 osteoarthritis of my major joints, I can report that I skied for a week in Vail this past February as I did a year ago, recently spent three days wading though spring creeks in Southwestern Wisconsin with a fly rod in pursuit of trout, and cycled 30 miles last Saturday. I am not alone as my biking, skiing and cycling buddy with similar knee issues returned last week from his yearly helicopter skiing adventure. I have been managing his knee arthritic issues with regenerative medicine interventions for over five years.
Then there are the athletes in their 50s. Certainly, the option is there for a joint replacement for a grade three arthritic joint but what If? What if there is a complication, an adverse event, a failure to regain motion, or residual pain? The fall back potion after a failed joint replacement is another joint replacement and the outcomes of revision surgery are frequently not satisfactory. Several weeks ago, I described the recreational pursuits of a 58-year-old volleyball enthusiast who had initially considered a joint replacement when 15 years after an arthroscopic partial meniscectomy, the predictable post traumatic arthritis had forced him to suspend his activities. He chose a regenerative medicine stem cell option; and eight weeks thereafter, he is back to playing volleyball three times a week. While on occasion, a booster follow-up injection is needed; we are in the process of developing a manuscript for scientific publication focusing on the successful outcomes of 20 patients followed for one to two years after a combined injection of bone marrow concentrate containing stem cells into the knee and the bone adjacent to the knee. These are recreational athletes between ages 45 and 60 who won’t quit.
On May 4, I am one of three invited faculty to present at The Regenerative Medicine Training Institute (RMTI). On June 7 and 8, I have been asked to participate in the Workshop and Lab Faculty at the largest Regenerative Medicine program in North America (TOBI). Owing to our integration of patient care with scientific outcomes monitoring, we have been able and continue to provide masterful and evidence-based care to aging athletes. To continue to remain in the forefront of Regenerative Medicine, I dedicate a good deal of time reviewing the future while monitoring the outcomes of patient care. Several new treatment options are soon to be launched including expanding my scope of care to those with inflammatory arthritis.
To learn more, call for a consultation (312) 475-1893. You may visit my website: www.sheinkopmd.com
Tags: ACL, ACL Injury, anterior cruciate, arthritic knee, arthritis, Autologous Protein Concentrate, baseball, BMC, board-certified, Bone Marrow Concentrate, bone marrow edema, cells, cellular orthopedic, cellular orthopedics, FDA, football, golf, Growth Factors, hematopoietic cell, injection, Interleukin 1 Receptor Antagonist Protein, IRAP, joint health, joint pain, knee replacement, lipogems, meniscal injury, meniscectomy, Mesenchymal Stem Cell, micro-fragmented adipose, muscle injury, muscle strain, OA, Orthopedic Surgeon, Osteoarthritis, pain, Physical Therapy, Platelet Rich Plasma, platelets, PRP, regenerative medicine, repair, Rotator cuff tear, soccer, sports injuries, sports medicine, stem cells, strain, tear, torn medial meniscus, training, volleyball
Apr 4, 2019
A patient presents to the office because of pain in the knee with or without a history of injury. An examination is performed followed by an X-Ray. Osteoarthritis may or may not be seen on the X-ray. If there is an altered range of knee motion when compared to the “normal” side, then a preexisting condition is considered. Whether or not the physician considers arthritis, an MRI is requested. The MRI report 48 hours after imaging is consistent with a torn medial meniscus. Should all patients with a torn medial meniscus undergo surgical intervention? If surgery is undertaken, should the procedure be a repair or a partial removal? The management of meniscal injuries must be influenced by the knowledge that meniscal integrity is important in load distribution across the joint. Meniscal injury causes altered joint mechanics and is related to the onset of arthritis.
According to a recently published online article in the British Journal of Sports Medicine, arthroscopic partial meniscectomy (APM) may not be the best option for all patients with knee pain and meniscal tear. Researchers investigated patients with meniscal tears that compared Arthroscopic Partial Meniscectomy to nonsurgical intervention, pharmacological intervention, and no intervention. At six to 12 months, APM patients had a slight improvement in knee pain, knee-specific quality of life, and knee function compared to physiotherapy patients. When excluding osteoarthritis (OA) patients, the aforementioned outcomes exhibited small to moderate improvement. Knee pain, function, and quality of life did not improve for APM patients compared to placebo surgery patients at six to 12 months regardless of OA status.
There may, however, be a small-to-moderate benefit from APM compared with physiotherapy for patients without osteoarthritis and who have mechanical or obstructive signs. Arthroscopic partial meniscectomy (APM), a keyhole surgery where loose and fragmented pieces of a torn meniscus is removed, is one of the most common orthopedic procedures performed. Over half of these are performed to treat a meniscus tear in a degenerative knee; however, several recent randomized trials have shown that Arthroscopic Partial Meniscectomy is not superior to conservative treatment or placebo treating meniscus tears associated with a degenerative knee. On the other hand, there is universal agreement that the traumatic meniscus tear, the result of a knee injury in a younger patient with otherwise healthy knee (with no degeneration), should be treated by surgery.
Then what is the downside of meniscal injury and surgery? The medial and lateral meniscus together provide shock absorption, establish a broad base of contact surface and help provide stability to the knee. Those who have undergone total or partial meniscectomy should understand that in five to 15 years, they will develop degenerative arthritis. The long-term outcomes of those whose tears were treated by repair rather than removal has not been established. My Regenerative Medicine practice in part, is the result of those seeking to postpone or avoid a Total Knee Replacement years after a meniscal injury followed by arthroscopic surgery. As long as the arthritis has not progressed to a Grade 4, I am able to assist the patient with joint restoration, at times joint regeneration, it is matter of age and health. While I am able to offer joint restoration, on occasion, joint restoration for those who sustained meniscal and Anterior Cruciate injury in the past, is there anything that could be used as an adjunct at the time of the meniscal injury to promote healing without surgery or postpone, perhaps avoid future postraumatic arthritis?
To learn more. Schedule a consultation (312) 475-1893.You may view my web site at www.sheinkopmd.com.
Tags: ACL, ACL Injury, anterior cruciate, arthritic knee, arthritis, Autologous Protein Concentrate, baseball, BMC, board-certified, Bone Marrow Concentrate, bone marrow edema, cells, cellular orthopedic, cellular orthopedics, FDA, football, golf, Growth Factors, hematopoietic cell, injection, Interleukin 1 Receptor Antagonist Protein, IRAP, joint health, joint pain, knee replacement, lipogems, meniscal injury, meniscectomy, Mesenchymal Stem Cell, micro-fragmented adipose, muscle injury, muscle strain, OA, Orthopedic Surgeon, Osteoarthritis, pain, Physical Therapy, Platelet Rich Plasma, platelets, PRP, regenerative medicine, repair, Rotator cuff tear, soccer, sports injuries, sports medicine, stem cells, strain, tear, torn medial meniscus, training, volleyball

Oct 5, 2018
After reviewing a CT scan of the right knee where a Total Knee Replacement had been done provided by a patient who sought my opinion for stem cell treatment of her arthritic left knee, I called her to discuss the possible reasons that the right Total Knee Replacement that she had undergone over ten years ago was never satisfactory. At the time of the right TKR for arthritis, she had elected for what seemed at the time as a logical intervention for a painful, arthritic, right knee. The outcome was at first complicated by a lot of postoperative swelling and pain; at one-year post-operative, the patient had never been pain-free nor had she ever regained her preoperative range of motion and that adverse outcome has persisted for over ten years. Fast forward a decade and the right knee has continued to be a source of pain and limited motion; so much so that the patient decided to seek consultation for a Stem Cell treatment for her now arthritic left knee.
Her first question was basically “does stem cell therapy for knees work?”. Our data collected on patients treated in this office over the past six years, since I started my practice, is compatible with an 85% patient satisfaction rate. We have not recorded one complication. To be forthright, not every patient has a perfect result; but the vast majority experience marked reduction in pain, increased motion and a significant improvement in functional capacity. Unlike a failed outcome of a Total Knee Replacement, our stem cell injections may be repeated at anytime if the benefits of the initial intervention do not last.
When it comes to the cost of a stem cell intervention, while the Total Joint Replacement is more often than not covered by some type of insurance, our fee schedule is in keeping in line with the deductible a patient has to pay out of pocket for the major surgery. If you do the math and additionally compare the risks and benefits of a stem cell intervention with a total knee replacement, you will note:
- Remote to little risk of complication with a stem cell procedure
- Comparable cost comparing my charges for a stem cell intervention with the inherent deductible obligation for a Total Joint Replacement
- Rapid recovery with a stem cell intervention versus the risks of an adverse outcome as experienced by the patient seeking consultation for stem cells
To seek consultation call (312) 475-1893. You may visit my website at WWW.sheinkopmd.com
Tags: cellular orthopedics, ct scan, joint health, joint replacement, knee pain, knee replacement, Osteoarthritis, regenerative medicine, stem cell treatment, TKA
Jul 19, 2018
The argument frequently advanced by orthopedic surgeons in response to a patient’s inquiry concerning stem cells for arthritis is that it is too early, there is not enough research, It is better to have a major surgical procedure. For those of you who have read my blog or have sought orthopedic consultation in my office, I have emphasized that my recommendations are evidence based. Each patient, for whom I have completed a cellular orthopedic intervention for arthritis, has been entered into a registry or clinical outcomes data base, IRB approved. Just as I pioneered the integration of clinical care with clinical research over 37 years as a joint replacement surgeon, so too do I now partake in the growth and development of the clinical pathways for regenerative medicine.
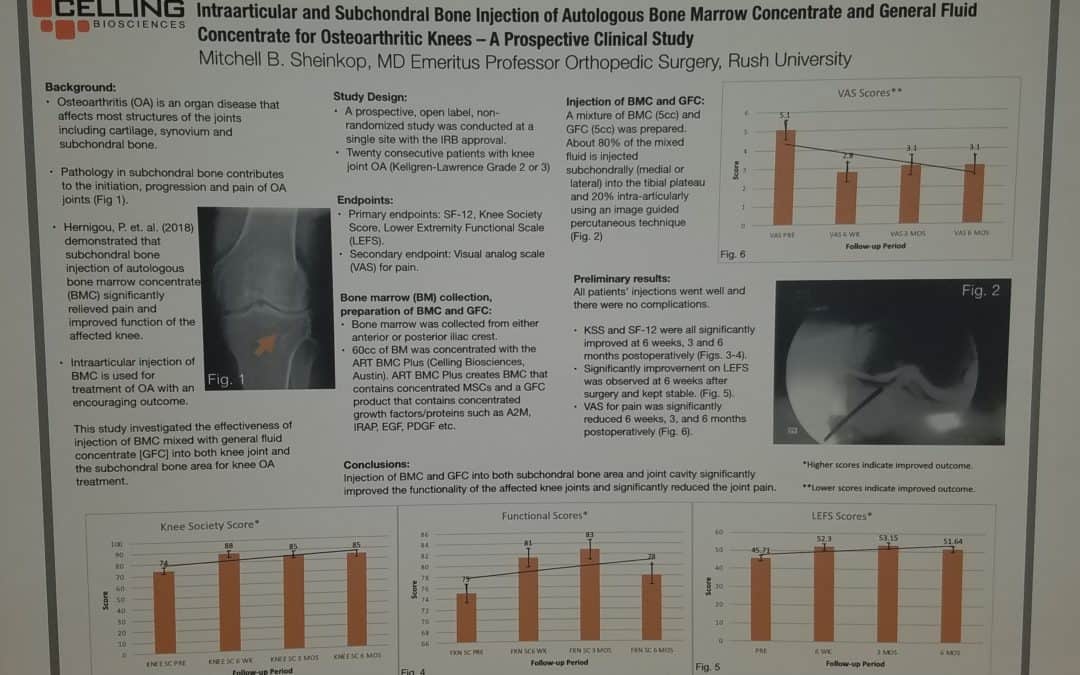
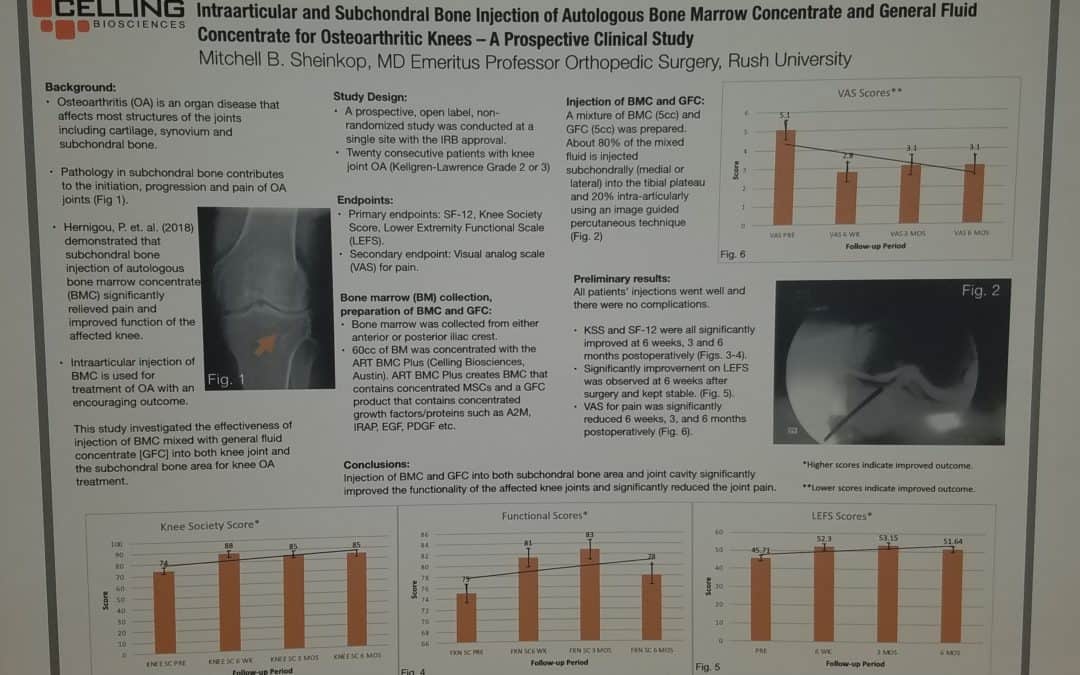
Last month, I exhibited a poster at a large regenerative medicine meeting wherein I shared my preliminary outcomes and thus educated other professionals using Intraarticular and Subchondral Bone Injection of Autologous Bone Marrow Concentrate and General Fluid Concentrate for Osteoarthritic Knees-A Prospective Clinical Study. Osteoarthritis is an organ disease that affects most structures of joints including cartilage, synovium and subchondral bone. Pathology in subchondral bone contributes to the initiation, progression and pain of Osteoarthritis. In previous European studies, the injection of autologous bone marrow concentrates into bone supporting the joint significantly relieved pain and improved function of the affected knee. The preliminary outcomes in the study that I presented via a poster exhibit, investigated the effectiveness of injections of Bone Marrow Concentrate with General Fluid Concentrate (Growth factors), into both the knee joint and the subchondral bone. The study recorded all the standard Endpoints I had previously used in joint replacement clinical outcomes trials.
Bone Marrow was collected from the pelvis and a filtration system allowed for concentration of Mesenchymal Stem Cells, Platelets, Precursor Cells and Growth factors such as A2M, IRAP, EGF, PDGF, TNF-B blocker, etc. After preparation, a mixture of Bone Marrow Concentrate and Growth factor Concentrate was injected into the bone (subchondral) and into the joint.
In the study, all patient injections went well and there were no complications. The Preliminary Results documented diminished pain and improved function. We concluded that injection of Bone Marrow Concentrate and Growth factor Concentrate into both the subchondral bone area and joint cavity significantly improved function of the affected knee joints and significantly reduced joint pain. While there are many stem cell providers to be found because of their marketing, choose the center of excellence in Cellular Orthopedics that is evidence based.
Call to schedule a scientific based consultation from an orthopedic surgeon 1 (312) 475-1893.
You may access my web site at www.SheinkopMD.com.
Tags: avascular necrosis, bone lession, bone marrow, Cartilage, cellular orthopedics, clinical study, Growth Factors, IRAP, joint pain, joint replacement, knee pain, knee replacement, meniscus tear, Osteoarthritis, platelets, PRP, regenerative medicine, sports medicine, stem cells, subchondral bone